Your cart is currently empty!
Short leg syndrome (part 1)
Leg length discrepancy, or as it has been alternatively termed, the SHORT leg syndrome, is by far the most IMPORTANT postural asymmetry. Limb length discrepancy is simply defined as a condition where one leg is shorter than the other.
If a substantial difference exists, disruptive effects on gait and posture can occur.
Leg-length discrepancy can be divided into two etiological groups:
- Structural. True shortening of the skeleton from congenital, traumatic or diseased origins.
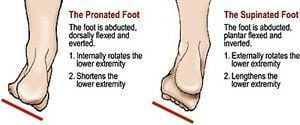
- Functional. Development from altered mechanics of the lower body, such as foot hyperpronation/supination (Figure 1), pelvic obliquity, muscle/joint imbalances, poor trunk stabilization and deep fascial strain patterns.

Faulty feet and ankle structure profoundly affect leg length and pelvic positioning. The most common asymmetrical foot position is the pronated foot. Sensory receptors embedded on the bottom of the foot alert the brain to the slightest weight shift. Since the brain is always trying to maintain pelvic balance, when presented with a long left leg, it attempts to adapt to the altered weight shift by dropping the left medial arch (shortening the long leg) and supinating the right arch to lengthen the short leg.1 Left unchecked, excessive foot pronation will internally rotate the left lower extremity, causing excessive strain to the lateral meniscus and medial collateral knee ligaments.
Conversely, excessive supination tends to externally rotate the leg and thigh, creating opposite knee, hip and pelvic distortions.
Arch Adaptations
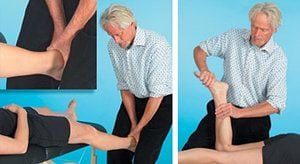
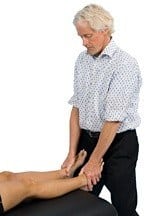
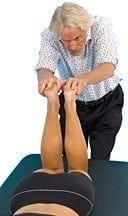
Most structurally oriented bodyworkers have learned hands-on routines for separating adhesive fascial bags of the 11 lower leg muscles to lift (or lower) dysfunctional foot arches. To insure proper foot functioning, tone must be stimulated in weakened arch muscles using fast paced muscle spindle techniques. As the myofascia regains lost elasticity, blood flow and vital nutrients permeate the fatigued tissues, allowing the muscles of supination (tibialis anterior, peroneus longus, tibialis posterior, etc.) to regain strength and mobility. In addition to myofascial work, one also must focus on restoring alignment and motion to the subtalar joint commonly stuck in a valgus (pronated) position (Figure 2). The subtalar or talocalcaneal joint forms the articulation where calcaneus and talus meet and allows foot inversion and eversion. To restore normal subtalar alignment, the therapist decompresses, abducts, plantar flexes and inverts the foot using myoskeletal contract-relax-assist (CRA) maneuvers. After successfully mobilizing the talus and calcaneus, all remaining ankle and foot joints should be systematically assessed and corrected.
Biomechanical Relationship of Feet to Pelvis
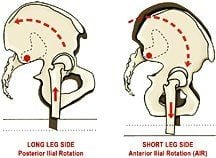
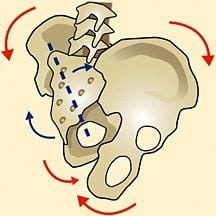
Coupling of Ilial Rotation and Leg Length Discrepancy. (Adapted from Mitchell F. Jr. The Muscle Energy Manual with permission)
Ilial rotation is coupled with leg length discrepancy. In Figure 4, the femoral head on the long leg side “drives” the ilia upward and backward. Conversely, the ilium on the low femoral head side drops down (anteriorly rotates). The concurrent rotation of both ilia in opposite directions produces a left-on-left sacral torsion (Figure 5). This complex ilial rotation coexisting with sacral rotation usually is described as pelvic obliquity. Weight bearing on the right leg will produce this common compensatory pelvic pattern. Ilial rotation can be palpated by placing your fingers under each ASIS and shifting weight from one leg to another. Now place your thumbs on each sacral base and shift side to side. Right leg weight-bearing should cause the right sacral base to go deep (anteriorly rotate).
Locomotion
(Adapted from A Quinn with permission).
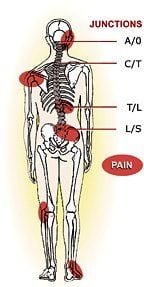
For efficient locomotion, a symmetrical and well-aligned body is essential. When the three bones of the pelvis are distorted by limb length discrepancies, gravitational forces wreak havoc on weakened SI joint and accessory pelvic ligaments (sacrotuberous and iliolumbar). These structures find themselves desperately struggling to maintain structural balance. Left untreated, a diverse array of symptoms appears as the SHORT leg destabilizes the pelvis by unleveling the sacral base. Painful lumbar compensations often travel all the way up through the atlantooccipital (A-O) joint, as the spinal column is forced to rotate and side-bend to accommodate the uneven sacral base.
In the lower limbs, short leg compensations can be summarized as follows:
- Ankle instability due to foot supination on the short side;
- Knee hyperextension on the short side and the knee flexed on the long side;
- Externally rotated leg on the short side; and/or
- Circumduction of the long limb.
Trunk and Head Compensations
Compensatory (functional) scoliosis commonly is reflected as a low shoulder on the high ilium side, as seen in Figure 7. A short “C” curve is common in the cervical spine, due to a “stuck” occipitoatlantal joint unable to tilt the head on the neck to level the eyes with the horizon. Elbow and hand positions can appear shorter on the short leg side, with the opposing arm swinging more on that side. Some authors suggest that there is a rotation of the pelvis toward the long leg side, possibly due to hyperpronation and medial leg rotation.2 These authors describe a typical gait when the short leg steps down and the long leg compensates by “vaulting.”
Walking on the toes on the short side and flexing the knee of the long side seems to be a fairly consistent compensatory movement pattern. As the center of gravity unevenly shifts, the smooth sinusoidal motion of gait is disrupted. Thus, the COSMETIC effect of walking also can contribute to the compensatory mechanism and eventual injury. For example, walking on the toes can lead to contracture of the Achilles and calf muscles, creating conditions such as Achilles tendinitis and plantar fasciitis.
Other functional scoliotic compensations include shortening of the quadratus lumborum on the long side, and a shortening of scalene, levator scapulae, sternocleidomastoid, and upper trapezius muscles on the contralateral side. This typical adaptive muscle imbalance pattern helps maintain erect head position with eyes level. Regrettably, prolonged muscle shortening “crams” vertebral and rib articulations, compounding the problem. The spine’s neuronal pool overflows as subthreshold stimuli progress to full-blown efferent nerve discharge, triggering increased muscle guarding. Thus, a vicious pain/spasm/pain CYCLE sinks its neurological tentacles deep into old intrinsic spinal groove muscles (rotatores, multifidus, intertransversarii and levator costalis), resulting in central nervous system overload, limbic system hyperactivity … and dis-STRESS.
The presence of a limb length discrepancy usually is easily recognizable during gait by observing the following:
- Shoulder tilting to one side;
- Inequal arm swing;
- Pelvic tilt;
- Foot supinated on the SHORT side and pronated on the long side;
- Ankle plantarflexed on the short side; and/or
- Knee flexed on the long side.
Note: During running, it has been suggested that limb length discrepancy makes no real difference, due to the fact that only one foot strikes the ground at any given time. However, Blustein and D’Amico’s extensive research finds that leg length discrepancy is the third most common cause of running injuries.
Summary
The IMPORTANCE of limb length discrepancy cannot be ignored and often is the key feature in lower limb and back pathologies. Thus, the use of proper visual and anatomic landmark evaluations is paramount in distinguishing between a functional and a structural limb length discrepancy. If in doubt about your ability to adequately and consistently distinguish leg length differences, have a three-dimensional radiographic postural study performed by a qualified manual medicine physician.
Proper limb measurement is essential. Unfortunately, there is no single hands-on method proven completely reliable in its own right. It is for this reason that therapists should develop a holistic approach that includes systematically eliminating aberrant lower limb myofascial strain patterns while restoring joint play to all feet and ankle bones. Although presentations do differ from client to client, most of the previously discussed patterning theories will prove accurate. During the assessment phase, the most important feature for the beginning therapist to recognize is that asymmetry exists. From there, more specific details emerge with experience.
Integral parts of treating the condition are identification, comprehension of each individual’s compensatory adaptations and their relationship to resultant symptomatology. Today’s touch therapist must be aware of the fundamental IMPORTANCE of limb inequalities, particularly the “short right leg” controversy featured in my next column.
References
- Donatelli R. The Biomechanics of the Foot and Ankle. F A Davis Co., 2006; pp. 55-9.
- Blake RL, Ferguson H. Limb length discrepancy. JAPMA, 1992; pp. 33-8.
- Blustein SM, D’Amico JC. Limb length discrepancy: identification, clinical significance and management. JAMPA, 1985; pp. 200-6.
By Erik Dalton, PhD
Short Leg Syndrome (part 2)
right leg.
A highly debated postural issue begging for a logical explanation is the “short right-leg syndrome” (Fig. 1). Although an inferred awareness of right-sided limb-length shortness has existed for centuries, along with decades of published research, no one has provided a universally acceptable answer to two very important questions:
- Why the unusual frequency of short right legs seen in clinic?
- How does this common postural pattern cause compensatory hip, back and pelvic pain?
Let’s begin by reviewing notable research regarding functional and structural short right legs and then discuss theories, assessments and corrections that help deal with this troublesome disorder.
As Sir William Osler once stated, “In order to treat something, we must first be able to recognize it.” Any attempt to tackle limb-length discrepancy and associated compensations, armed with inadequate evaluation tools, surely will lead to failure and frustration. In the absence of radiographic measurements, massage therapists must develop keen palpatory and visual skills for detecting osseous and soft-tissue dysfunction. Aberrant patterns are best identified and classified using the acronym ART: Asymmetry, Restriction of motion, and Tissue-texture abnormality. Although numerous tests and treatment modalities have proven successful in treating short legs and associated compensations, we’ll focus on only a few fundamental myoskeletal techniques that add to your toolbox of touch.
Leg Length and Back Pain
In two exquisitely designed studies (1962 and 1983), Denslow and Chase measured leg-length discrepancy in 361 and 294 subjects presenting with low back pain. Using the most advanced radiographic technology currently available, their papers (published in the American Academy of Osteopathy) reported the following findings concerning limb-length discrepancy:
- Significant incidence of short right legs (66 percent);
- Lumbar convexity to the short leg side (side bent left – rotated right); and
- A high correlation depicting contralateral (left) pelvic rotation.(Fig. 2)
By comparing sagittal-plane femoral-head height and sacral base angulation (Fig. 3), the authors concluded that innominate bones rotate around the sacrum (iliosacral tilt). Transverse plane images revealed that the pelvis also can rotate as a block around the vertical lumbar spine. Denslow and Chase’s pioneering work helped biomedical researchers understand how shortened limbs torsion the pelvis, creating painful lumbar compensations. Their data not only confirmed leg-length findings conducted by previous researchers but also prompted new, more sophisticated imaging studies. In 2004, John H. Juhl, DO, reported that 68 percent of 421 low back pain patients presented radiographically with short right legs.
Functional Leg-Length Assessments
Through the years, manual therapists have developed many creative ways to differentiate functional (fixable) from structural (true) limb-length differences. Screening exams taught in educational programs often place too much emphasis on supine leg-length assessment in determining pelvic disorders. Commonly, one leg will appear shorter during visual observation of the supine client’s medial malleoli (Fig. 4) when, in fact, the leg lengths actually are equal or just the opposite of how they appear radiographically when standing. For example, in the presence of a true (structural) short right leg, standing ASIS measurements should show an inferior slope on the short side. However, when the client lies supine (removed from vertical gravitational compression), the left leg may suddenly test shorter than the right.
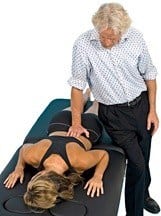
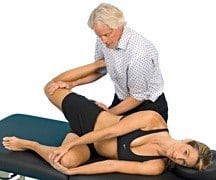
While many factors may contribute to this finding, one of the most common culprits is length/strength imbalance in deep intrinsic postural muscles such as the quadratus lumborum (QL). When unilaterally short and tight, the QL can ‘hip hike’ the left ilium as the client assumes an off-weighted supine posture. Confusion mounts as the left leg now appears shorter than the right. Figure 5 presents an effective contract/relax/assist manoeuver to lengthen the hypercontracted left QL.
Fig. 5 presents an effective contract/relax/assist manoeuver to lengthen the hypercontracted left QL. Although leg, hip and pelvic corrections shouldn’t be based solely on supine test results, helpful information is derived by combining it with other exams such as prone leg-length tests. These oft-neglected prone assessments offer therapists additional clues for solving the limb- length puzzle. When prone, both ASISs are “pinned” to the table, thus preventing ilial rotation and allowing the therapist to isolate sacroiliac and axial skeletal joint dysfunction.
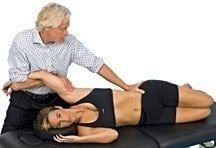
to lengthen tight/short left QL.
Here’s a quick reference for differentiating supine from prone limb-length assessment:
- Supine: Tests leg-length differences resulting from iliosacral rotation, typically due to muscle imbalance.
- Prone: Tests leg-length inequality as the lumbar spine attempts to adapt to sacral-base unleveling in the presence of SI joint dysfunction.
Depending on the degree of leg-length shortness, compensations may travel all the way up through the cervical spine and into the cranium (Ascending Syndrome). Conversely, “key” restrictions sometimes begin in the head or neck and travel down the kinetic chain (Descending Syndrome), causing pelvic obliquity and adaptive leg-shortening (Figs. 6A and B).
During the course of an examination, several simple tests help uncover the biomechanical root of the shortened leg. However, none are adequate to fully assess all possible causes. The Derifield (deer-field) Maneuver3 and others discussed below are useful in “weeding out” spinal and pelvic disorders.
The neurological basis for body balance is found in the brain’s reticular system, where the inhibitory and faciliatory systems maintain muscle balance. Cranial or cervical fixations can affect lower-limb musculature via tonic neck reflexes, resulting in the appearance of one leg being SHORT when viewed with the client in the prone position. Typically, comparisons are made by observing the feet, with knees in extended and flexed positions, noting any leg- length disparity (Fig. 7).
To determine if head/neck restrictions might be altering leg length, the therapist places the thumbs inferior to the medial malleoli. The client is asked to turn their head to one side and then the other. If cervical joint restrictions and/or bony spurs “snag” the dural membrane, head-turning can twist and torsion the sacrum, resulting in leg-length changes. Sometimes, the apparent leg-length discrepancy is resolved or even reversed during these cervical rotation manoeuvers.
Note: If left side head rotation causes the legs to become equal, the therapist should label this as a positive left cervical syndrome and proceed to evaluate and correct all motion-restricted cervical segments (including the O-A joint) that could be dragging the dura and shortening the leg.
The second phase of testing begins with the client’s head in neutral with the therapist’s thumbs evaluating medial malleoli height. Once a visual measurement has been noted, the therapist’s hands slightly plantar-flex the client’s feet while slowly bending the knees to 90°, examining for any changes in heel height.
The Derifield Maneuver
Four possible findings may be noted during this test:
- Short leg stays short. If one leg is anatomically short, no change in leg length should occur as the knee moves from extension into flexion (Fig. 8). Referral for foot orthotics may be necessary.
- Short leg gets shorter. Sacroiliac and lumbar spine dysfunction can create muscle hypertonicity that shortens the leg in appearance as it is flexed. Figures 9A and B show effective myoskeletal springing maneuvers for derotating the pelvis to correct sacroiliac and lumbar spine asymmetry.
- Short leg becomes longer. A posteriorly rotated and fixated ilium (usually left) shortens the leg. When accompanied by an adhesive right-anterior hip capsule, increased rectus femoris pull during knee flexion shortens the right extremity causing the left leg to appear as long, or longer, than the right. This is termed cross-over. * The therapist should perform spring tests for a posteriorly fixated left ilium and anteriorly fixated, right hip capsule (Figs. 10A and B).

- Heel Drop: With knees flexed 90°, the therapist allows both heels to drop toward the buttocks to see if one leg falls farther than the other. The HEEL falling farther usually is a positive indicator of a posterior sacral rotation on that side. This finding is noted as a positive Webster’s sign.4 A variety of spring tests can be used to identify and correct the torsion.
Neurological Explanations for Short Legs

When a short-right-legged client stands with each foot resting side by side on bathroom scales, a measurable weight-shift typically occurs to the low side. The Leaning Tower of Pisa demonstrates this normal law of physics. However, the Tower does not possess a nervous system. Several researchers including Kappler, Previc and Pope5,6,7 believe that some individuals unconsciously resist this gravitational pull by sideshifting body weight to the left side, through a prenatal organizational system called cerebral lateralization. Their research theorizes that motor dominance overrides anatomical and gravitational factors in these individuals. It’s thought that right motor dominance has roots in fetal positioning during the third trimester, resulting in the brain’s lateralization process.
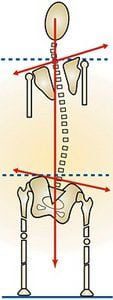
In the brain, motor dominance typically crosses cortexes from left to right (left brain controls right side of the body). Conveniently, left vestibular dominance, which assists in balance, coordination and orientation, travels ipsilaterally down the left leg to allow left-sided weight bearing during right motor-dominant activities. For instance, a right motor-dominant person typically balances on their left leg to perform tasks such as kicking a ball (Fig. 11). Combining right motor and left vestibular dominance often results in a left-sideshifting maneuver of the pelvis over the vestibularly long left leg during standing (Fig. 12). This neurological postural shift helps explain many unusual pain patterns seen in clinic.
Short Leg Symptoms
Those with short right legs who bear more to the short right side usually report greater SI joint pain in the right hip and low back area. Examination of the sacrum often reveals a deep right sacral base, positive spring test for anteriorly fixated ilium and tender iliolumbar and sacroiliac ligaments. Conversely, motor-dominant clients who side-shift over the left leg usually experience greater left-sided SI joint pain and a positive spring test for a posteriorly fixated ilium. Symptoms worsen during prolonged walking or running, as overstretched abductors grind against the greater trochanter, creating bursitis, gluteus medius tendinosis and piriformis syndrome.
Since the human body rarely is symmetrical side to side, testing for loss of joint play often provides more reliable information than analyzing anatomical landmark findings. For decades, therapists have utilized spring tests to determine the presence (or absence) of joint play in ankles, feet, hips and shoulders. Regrettably, spring tests are not as commonly used to evaluate spinal and sacroiliac joints. Therapists can benefit greatly by observing for common postural patterns during gait, checking anatomical landmarks, and spring testing questionable structures to see if the findings have relative value. Iliosacral, SI joint, and lumbar spine spring tests are valuable assessment and treatment TOOLS that fit perfectly into a massage therapy format. Following the supine and prone leg-length tests, specific springing manoeuvers can be used to verify findings and correct motion-restricted joints.
Since SHORT limbs arise from biomechanical as well as neurological factors, therapists must take time to fully evaluate the client looking for common compensatory patterns such as the short right leg. Visual observation of the client’s gait alerts the therapist to the possibility of cerebral lateralization and accompanying pelvic side-shifting. Supine and prone exams should be compared with other anatomical landmark findings to determine whether iliosacral, sacroiliac or head and neck restrictions are responsible for limb-length problems. Discrepancies greater than 2 cm can be associated with scoliosis, pelvic obliquity and alterations in the normal walking cycle. From a functional standpoint, there is strong, though not conclusive, evidence of an associated increase in the incidence of low back pain and hip joint osteoarthritis.
References
- Denslow J, Chase I, et al. Mechanical stresses in the human lumbar spine and pelvis. In: Postural Balance and Imbalance. Peterson B, ed. Indianapolis: American Academy of Osteopathy, 1983, pp. 76-82.
- Juhl J. Prevalence of frontal plane pelvic postural asymmetry. J Am Acad Osteopath Assoc, October 2004;104(10):411-21.
- Cooperstein R. The Derifield pelvic leg check: a kinesiological interpretation. Chiropractic Technique, 1991;3:60-65.
- Bovee ML. The Essentials of the Orthopedic & Neurological Examination. Davenport, IA: Palmer College, 1977.
- Kappler R. Postural balance and motion patterns. J Am Osteopath Assoc, May 1982;81(9):598-606.
- Previc FH. A general theory concerning the prenatal origins of cerebral lateralization in humans. Psychol Rev, July 1991;98(3):299-334.
- Pope R. The common compensatory pattern: its origin and relationship to the postural model. Am Acad Osteopath J. 2003;14(4):19-40.
- Dalton E. Advanced Myoskeletal Techniques. Oklahoma City, OK: Freedom From Pain Institute, 2005, pp. 154-160.
By Erik Dalton, PhD
Welcome
Alfio Sorbello

Address
Room 3, Gold Coast Orthopedics
408 Coolangatta Road
Bilinga QLD 4225
Australia
Tel: 0414 356 567

Members Choice Provider

Recognised Partner


Featured Products
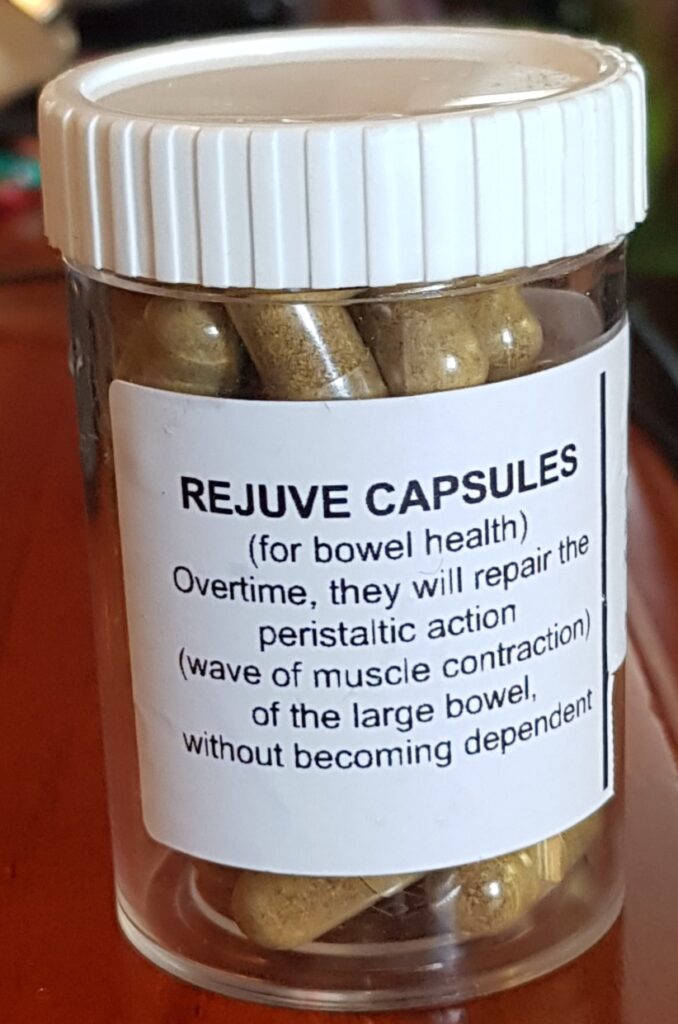
Life or Rejuve Capsules

Massage Gift Certificates (F) 60min